Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt's macular dystrophy: follow-up of two open-label phase 1/2 studies
Summary
Background
Since they were first derived more than three decades ago, embryonic stem cells have been proposed as a source of replacement cells in regenerative medicine, but their plasticity and unlimited capacity for self-renewal raises concerns about their safety, including tumour formation ability, potential immune rejection, and the risk of differentiating into unwanted cell types. We report the medium-term to long-term safety of cells derived from human embryonic stem cells (hESC) transplanted into patients.
Methods
In the USA, two prospective phase 1/2 studies were done to assess the primary endpoints safety and tolerability of subretinal transplantation of hESC-derived retinal pigment epithelium in nine patients with Stargardt's macular dystrophy (age >18 years) and nine with atrophic age-related macular degeneration (age >55 years). Three dose cohorts (50โ000, 100โ000, and 150โ000 cells) were treated for each eye disorder. Transplanted patients were followed up for a median of 22 months by use of serial systemic, ophthalmic, and imaging examinations. The studies are registered with ClinicalTrials.gov, numbers NCT01345006 (Stargardt's macular dystrophy) and NCT01344993 (age-related macular degeneration).
Findings
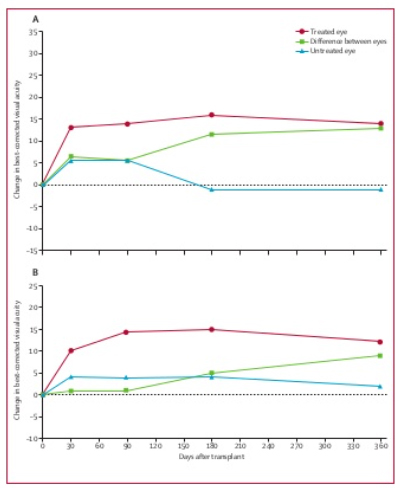
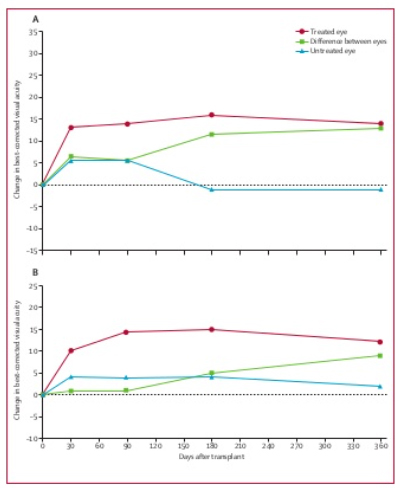
There was no evidence of adverse proliferation, rejection, or serious ocular or systemic safety issues related to the transplanted tissue. Adverse events were associated with vitreoretinal surgery and immunosuppression. 13 (72%) of 18 patients had patches of increasing subretinal pigmentation consistent with transplanted retinal pigment epithelium. Best-corrected visual acuity, monitored as part of the safety protocol, improved in ten eyes, improved or remained the same in seven eyes, and decreased by more than ten letters in one eye, whereas the untreated fellow eyes did not show similar improvements in visual acuity. Vision-related quality-of-life measures increased for general and peripheral vision, and near and distance activities, improving by 16โ25 points 3โ12 months after transplantation in patients with atrophic age-related macular degeneration and 8โ20 points in patients with Stargardt's macular dystrophy.
Interpretation
The results of this study provide the first evidence of the medium-term to long-term safety, graft survival, and possible biological activity of pluripotent stem cell progeny in individuals with any disease. Our results suggest that hESC-derived cells could provide a potentially safe new source of cells for the treatment of various unmet medical disorders requiring tissue repair or replacement.
Funding
Advanced Cell Technology.